


















Your time is valuable – depend on me to review options and recommend affordable premium choices to best meet your needs. As world-famous oil field firefighter Red Adair cautioned wisely: “If you think it’s expensive to hire a professional to do the job, wait until you hire an amateur.”
Souls on Board?
In most work settings, the onset or worsening of illness symptoms presents minimal challenge in getting to a setting for appropriate medical care. Coworkers often provide supportive care and summon assistance. Ambulances, usually staffed by Emergency Medical Technicians, play a vital role in the continuum of emergency care in almost all urban, suburban, or rural settings.
During automotive travel of any kind, the onset or worsening of illness symptoms can present more of a challenge, depending on whether the driver is the sole occupant and whether the distress is incapacitating or only mildly interferes with the ability to indentify and get to a nearby medical facility.
Air operations present entirely different and more ominous scenarios. Statistics are difficult to discover, but a minority of cross-country flights appear to be operated by a pilot as the sole occupant. Each of those instances, however. Is flirting with a disastrous outcome depending on a variety of uncontrolled circumstances. Every pilot can take reasonable preliminary steps to minimize the likelihood that health or medical emergencies arise during the course of a flight.
Links in the Chain to “Pan – Pan” or “Mayday”
A common method of evaluating aircraft accidents is to review the series or “chain” of events and decisions starting with the first departure from best practices. If at any point leading up to the accident a “link” is broken by a sound decision, an accident can be prevented. Emergency declarations during cruise are most commonly thought of as relating to aircraft system malfunctions, such as engine failure, fuel starvation or exhaustion, avionics or electrical power failure, communication or navigation equipment failure, detection of smoke or fumes or fire, structural issues related to bird (or drone?) strike, or unexpected weather encounters. These circumstances can mean that your aircraft is in a state of distress, usually where imminent danger means you require immediate assistance to aid in safely landing. Being “lost” or otherwise unsure of a variety of circumstances is not commonly considered as a priority but such situations do compromise conduct of the flight.
Urgent conditions can quickly progress to more serious “emergency” events. posing rising risks to survival. In every one of these scenarios, various pre-planning and pre-flight checklists are embedded with inquiries and inspections to minimize risks or to help optimize the available resources for safe conclusion of the flight. Controlling facility personnel can be invaluable in safe resolution of most emergencies. [Best ways to contact Air Traffic Control: (1) Announce your plight “on frequency” during IFR flight or VFR Flight Following; (2) Announce on Guard frequency 121.5 MHz; (3) Announce (“Any aircraft”) on any recent frequency (or CTAS for a nearby airport, such as 122.8 MHz); (4) Announce on Flight Service frequency (such as 122.2 MHz, maybe 122.4 or 122.6 locally) … and even dial “7700” on your transponder to alert ATC]
One area to which less attention is given in training involves gradual or sudden physical impairment of the often-solo pilot. The “IM SAFE” and other checklists can be casually overlooked but they are designed to identify and mitigate evolving risks associated with the operator not the aircraft.
Dire Straits (Pilot Incapacitation)
As noted on Skybrary.aero, “Pilot incapacitation is the term used to describe the inability of a pilot, who is part of the operating crew, to carry out their normal duties because of the onset, during [any phase of] flight, of the effects of physiological factors.”
“Fitness for flight” is the FAA term for establishing medical certification standards and cautionary guidelines regarding illness, medications, alcohol, and other impairing conditions. Among these, fatigue is most prominent, followed by stress and then emotional factors. During flight, hypoxia is a real threat, followed by ear block, sinus block, decompression after scuba diving, hyperventilation, carbon monoxide poisoning in flight, visual illusions, and visual changes in dim or bright light. While G forces are expected with aerobatic flight, challenging sensory impairment can occur with position changes of your head, such as frequent or prolonged study of a tablet EFB, map, or other documents. If control of your aircraft has digressed to where your flight path becomes erratic, G forces can be a real risk then.
A brief but thorough review of these factors is available in the Aeronautical Information Manual (AIM) published by the FAA:
https://www.faa.gov/air_traffic/publications/atpubs/aim_html/chap8_section_1.html
Of course, pilots of any age at any time can fall victim to health catastrophes, such as sudden cardiac events, seizures, strokes, sleep episodes, hypoxia, and acute pain syndromes. Timely identification and appropriate measures to mitigate risk can help to ensure flight safety. The FAA continues to monitor the prospect of pilot incapacitation during cruise flight and their significant risks to aviation safety:
For integrative medical approaches and helpful hacks to help address such profound medical concerns, CLICK on the diagnostic topics found in the lists on this website, on Page 2 – Pre-Check and Page 3 – Holding Short.

In grade school, we learn to limit our liquid intake because then we don’t have to leave in the middle of class to pee. That “education” carries forth for years: pilots of all experience and all varieties of aircraft are familiar dehydration … because drinking fluids means you’ve gotta “hit the head,” which can be challenging at altitude during cruise.
The low humidity levels in aircraft cabins contribute to dehydration, aggravated by longer flight times, often with the sun rays beating down, recent diuretic drinks (coffee, tea, alcohol, and “soft” drinks), excessive exercise, recent sunburn, improper attire for conditions, recent illness (especially with reduced thirst or diarrhea), and even effects of various medications. Dehydration associated with “heat stress” can cause headaches, dizziness, fatigue, cramps, sleepiness, reduced alertness and concentration, visual capabilities, dexterity, and impaired “caution and caring,” all affecting overall performance.
If a solo pilot fails to respond appropriately to heat stress, surviving the onset of progressive symptoms becomes ever more unlikely. Heat exhaustion (body temperature rising to 101-105 F) symptoms include worsening fatigue, nausea and vomiting, giddiness, cramps, and rapid breathing which creates more physiological stress, and fainting. Heat stroke, where body temperature exceeds 105 F, is uniformly fatal: heat control mechanisms fail, mental confusion and disorientation result in bizarre behavior and coma.
The risks are serious and the signals are subtle. Under certain conditions, external fluid replacement cannot keep pace with the loss of fluid, as with sweating or simple breathing. With excessive sweating, remember that you need additional salt not merely water. The Civil Aerospace Medical Institute of the FAA has an excellent review with guidelines for you to honor to stay safe and well:
“Dehydration and the Pilot,” https://www.faa.gov/pilots/training/airman_education/topics_of_interest/dehydration
Pilots are like everyone else, “gut” issues arise here and there. Irregular eating schedules and limited access to more appropriate food selections can place pilots at higher risk for suffering bloating, indigestion, constipation, even “urgency” or diarhhea, any of which can be distracting during flight. Higher altitudes can provoke bloating distress not usually seen on the ground.
In my lifelong career as an expert in integrative medicine, I have developed very successful approaches to resolving (or at least controlling) gastrointestinal issues. Almost all adults have suffered with these complaints, sometimes for years despite consulting dozens of doctors. If the “hacks” you can access by clicking above fail to provide expected relief, consider whether personalized consultation might be invaluable for your career and your future. You need to know that many (almost most!) disorders and diseases have their origin in your gut – is it time for you to finally get fixed?
Every pilot has heard of the dangers of hypoxia, where a deficiency if oxygen impairs tissue functions all over the body. The most worrisome symptoms involve your brain: impaired judgement, dizziness, reduced motor skills, and shortness of breath, posing significant safety risks. Failure to resolve this condition invariably worsens and is usually fatal for the solo pilot. Physical condition, altitude of your residence, breathing limitations (ease of breathing, reduced tidal volume), exercise conditioning, recent aggressive exercise, advancing age, lack of restful sleep, illnesses known and unknown, fluid retention, “fighting off” a cold, these and a wide variety of often recent factors influence your personal susceptibility but no one is immune to hypoxia episodes. Recurrent or prolonged exposures to hypoxia can injure brain and heart tissues, reducing your resilience for future episodes.
Respect for hypoxia is essential, because the results can be disastrous. The first recorded survivor of aviation-related hypoxia got to the nub of the problem when he described it as a seductive way to die. “‘One does not suffer in any way; on the contrary. One feels an inner joy, as if filled with a radiant flood of light,’ French pioneering balloonist, Gaston Tissandier, wrote in 1875. ‘One becomes indifferent, one thinks neither of the perilous situation nor of any danger.’” He was the only survivor of the first three French scientists who, according to the barometer in their balloon, reached 28,000 feet in 1875.
Staying alert to subtle hypoxia symptoms is challenging, since they often occur gradually and without obvious signals. Poor judgment expressed as a sense of wellbeing (euphoria) or irritability, headache, increased reaction time, impaired hand-eye coordination, drowsiness, dizziness, dimming visual acuity and narrowing peripheral vision (especially at night), restless agitation, tingling in fingers and toes, numbness, blue coloration of fingernails and lips, limp muscles or clumsiness, rapid pulse, chest tightness or even cough, and decreased memory or confusion or foggy decision-making or the ability to make calculations, and especially any combination of these is suggestive. Muscular coordination could be affected, such that even reaching for an oxygen mask might be difficult despite the desire. While symptoms vary from person to person, your own usually represent your “hypoxic signature,” the changes that you are more likely to express during the onset of any episode, consistent over time.
The Centers for Disease Control and Prevention have identified various risk factors that can aggravate “altitude sickness,” such as being overweight, sleep apnea, heart disease, lung disease (especially COPD or chronic obstructive pulmonary disease/emphysema), seizure disorders, and liver disease (cirrhosis and others).
Debilitating effects can occur without warning, with dramatically impaired pilot performance and loss of consciousness, perhaps as short as within 15 minutes at 15,000 feet MSL without supplemental oxygen. Sensory loss fades into semi-consciousness, unconsciousness, and after several minutes, death. The FAA Civil Aeromedical Institute reported a 1966 study where pilots were subjected to simulated oxygen levels for altitudes of 8,000, 10,000, and 12.500 feet MSL. Few problems were encountered in cruise flight. But in the descent that followed, when the oxygen-deprived pilots made significantly more errors, including misdialled radios, missed approaches, failure to follow ATC instructions, and one crash.
While sudden cabin decompression is sometimes thought to be a major factor, a U. S. military study found that 83 per cent occurred gradually and, with gradual hypoxemic symptoms, might not be readily recognized and resolved. One study emphasized the need to better understand the “combined effects of mild hypoxia with dehydration, sleep loss, long continuous working hours, and circadian dysrhythmia (jet lag), all of which are common in aviation.”
While private pilots generally flying below 10,000 feet MSL often consider that hypoxia is a minimal risk to performance, studies show that early symptoms can be detectable as low as 5,000 feet MSL. Normal blood oxygen saturation at sea level is about 21.9 per cent; at 5,000 feet MSL that can drop to 17.3 per cent. At 10,000 feet MSL, blood oxygen saturation can be down to 13.7. per cent. These reductions certainly can explain the many symptoms that can develop with hypoxia. At 15,000 feet MSL, the oxygen concentration in blood falls to 11.8 percent, almost half of that available at sea level.
Hypoxic hypoxia is where not enough oxygen is available to the body, such as at higher altitudes where the partial pressure is reduced. Oxygen in the air at 10,000 feet MSL is only about 70 per cent of that at sea level. Travelers above 8,000 feet MSL can experience “altitude thickness” from the “thin air,” sometimes needing 3 to 5 days to adjust. [For many years I’ve advised my patients regarding nutritional supplements that markedly reduce “jet lag” and “altitude stress.” – see the noted on “Click” above.]
Hypemic hypoxia exists where the blood cannot transport enough oxygen to the cells. Those with unsuspected anemia or other disease, recent blood loss (including donation), deformed cells such as with sickle cell, and heavy smokers (already internally at an altitude of 5,000 feet) or others with exposure to exhaust fumes are more at risk. Regarding aviation, carbon monoxide poisoning is the most common form, where hemoglobin in your red blood cells is irreversibly blocked (attaching 200 times more than oxygen) and cannot bind with and transport the continuing supply of essential oxygen. Carbon monoxide is odorless and a closed cabin can quickly become dangerous if an undetected leak continues from faulty equipment or malfunction of the muffler, the cabin heating system, or even through the firewall.
More rarely, stagnant hypoxia results from impaired or constricted circulation of your oxygenated, such as occurring due to excessive chilled environment or high G forces. Hyperventilation might be an early signal. Congestive heart failure (known or unknown) and blood clots (again, known or unknown) can be primary contributors.
Histotoxic (cell) hypoxia results when your body’s cells are unable to use oxygen efficiently. Alcohol and other drugs (especially antihistamines, tranquilizers, sedatives, and analgesics including narcotics) can reduce your otherwise satisfactory oxygen utilization. Cyanide poisoning is a classic example.
CFI Notebook has an excellent review of hypoxia with details:
https://www.cfinotebook.net/notebook/aeromedical-and-human-factors/hypoxia
Many people have experienced sharp ear pains, especially when descending from high altitude. This condition is aggravated when you have an ear infection or “cold” or other congestion, especially when sinuses or a “sore throat” are involved. Basically changes in pressure that are not readily equalized across your eardrum or in your sinuses can become suddenly painful and frustrating to resolve. The term “Eustachian dysfunction” describes where swelling from your throat to your eardrum can block the equalization of pressure. A deviated nasal septum (whether from injury or from birth) likewise can block pressure adjustments with sinuses. Sinus pains (even headaches) can be experienced around your eyes, behind your eyes, and even behind your ears. Holding your breath and bearing down can be successful to “pop” your ears, but that can put you at higher risk for infection. Swallowing repeatedly, chewing gum, and yawning can be effective and are safer simple attempts.
Decongestants, antihistamines, and “cold remedies” are readily available OTC (“over-the-counter”) and by prescription. Because various performance impairments can be significant, these are not generally approved for use by pilots, with certain drug exceptions designated by the Federal Air Surgeon. In my capacity as an Aviation Medical Examiner and as chief medial officer for Texas International Airlines, I advised airline pilots on a variety of safe ways to reduce and resolve ear and sinus co and ngestion problems. These “hacks” are available to you now when you “Click” above.
Some people suffer with seasonal or even chronic allergic congestion. Pilots might be fine “at home” but can be frequently and unexpectedly exposed to other symptom-provoking environmental conditions (trees, flowers, chemicals used in furnishings in overnight stays, different regions, different countries). Being ever vigilant to the sudden need for these effective “hacks” makes great sense, since pains from blocked ears or sinuses can be quite distracting.
Tooth ache or pain can be initiated or aggravated by changes in altitude (pressure). Want to impress someone? You can claim to be suffering from “aerodontalgia” or “barodontalgia,” otherwise known as flyer’s toothache. Typically pain will involve teeth that have had a recent history of trauma, cracked or chipped tooth, deep decay (cavity), deep fillings or crowns or root canal having been placed, infections, or other dental treatment. These teeth can have irritated nerves, with a suspicion of possible abscess occurring.
If a tooth has specific issue and you later experience barometric pain, upon landing symptoms of an abscess might occur, usually within 24 to 72 hours. Some dentists, upon being advised that you have an upcoming flight within a month of having deep fillings placed or a fractured/cracked tooth (with chewing symptoms) or a root canal, will offer a prescription of antibiotics and analgesics to be filled by a local pharmacy. Then the patient is asked to keep the prescription in their luggage, to be proactive in case a significant toothache develops, at which point they can immediately start the antibiotics. This helps to prevent having to seek the services of a dentist while traveling. Caution: potential use of antibiotics and especially analgesics (“pain killers”) must be carefully reviewed with your Aviation Medical Examiner, regarding their possible use and your performance of flight duties.
Maintaining good dental health, including having needed treatments, keeps you ahead of preventable problems. Staying well hydrated reduces discomforts that might arise. A cold compress can reduce immediate pain, and small ones are available if you anticipate the need.
My first book, on clotting systems, was written in 1971. Since then, medical diagnosis and care has advanced in wonderful ways but, sadly, many physicians fail to appreciate the likelihood and severity of developing DVT, deep vein thrombosis.
Deep vein thrombosis is a dangerous medical condition in which a blood clot forms in a deep vein, most commonly in the legs. The progression can vary: the clot may dissolve on its own, it can grow and extend, it can break apart and lead to serious complications. These can be life-threatening complications, such as a pulmonary embolism (PE), where the clot travels to the lungs. Depending on the extent and location, pulmonary embolism can result in death within minutes.
DVT is relatively common, with the Centers for Disease Control and Prevention (CDC) estimating that around 900,000 people in the U.S. are affected by DVT or PE annually. Of these, an alarmingly high number – approximately 60,000 to 100,000 people – die from complications related to these conditions each year. Early detection and treatment are crucial to prevent complications. Recognizing the symptoms and risk factors can help people seek timely medical attention and reduce their risk of more serious health issues.
Pilots are at special risk for developing DVT, due to prolonged sitting in a confined space, minimal ability to move their legs, and dehydration. Any hypoxemia (such as long hours at elevations above 5,000 feet MSL or more) can contribute as well. Several lifestyle factors can promote deep vein thrombosis: obesity, immobility, reduced activity, smoking, age over 50, and women more than men. Additionally, five percent of the population carries gene mutations (FVL and PGM) that can predispose one to the formation of clots. Pro-inflammatory foods (such as many called “fast foods”) can create physiology changes that tend more toward clots as well.
Heart disease, respiratory conditions, or inflammatory diseases like Crohn’s disease or ulcerative colitis may have a higher risk of DVT. Hormonal therapies, including birth control pills and hormone replacement therapy (HRT), can also elevate the risk of blood clots. A family history of DVT or PE can increase your risk at well.
Early recognition and appropriate medical treatment can be life-saving. Swelling occurs in about 70 to 80 per cent of patients with DVT, particularly in the calf or thigh, and is often one of the earliest and most noticeable symptoms. Tenderness with any pressure is present in about half of DVT patients. Cramping or aching pain is reported in some 50 to 60% per cent of cases, often localized to the calf, thigh, or foot. Pain might worsen when standing or walking and improve with rest, so you can easily mistake your discomfort for muscle soreness or a pulled muscle, so considering all of your symptoms becomes important.
Warmth in the affected area is experienced by around 40 to 50 per cent of those experiencing DVT. Some 30 to 40 pere cent could also see redness (“erythema”). Discoloration seen as a bluish or purplish tint to the skin, particularly in the lower leg, occurs in approximately 20 to 30 per cent of DVT patients. About one-third of those affected will notice tiredness or heaviness in the affected leg. Some 20 per cent could notice increasing prominence in the superficial leg veins. About 20 per cent could report sharp, sudden pain or muscle spasm or cramping in the calf or thigh. If localized dry or scaling skin changes are noted, as seen in about 10 per cent of patients, these might be signs of late-stage venous insufficiency and warrant urgent attention. Many people do not realize that deep blood clots can first form in the arch of your foot, feeling much like an unexplained “stone-bruise.” Be sure to present for immediate medical assessment as soon as possible after landing if you have suggestive symptoms.
Mobility is restricted on the flight deck, but flexing and relaxing your calf muscles every few minutes can help reduce your DVT risks. Remain hydrated, remain “walking active,” and pay attention to healthy habits such as getting enough restful sleep. Pilots who routinely fly long distances sometimes find more comfort in wearing stockings that provide mild compression. These and other valuable “hacks” are available to you now when you “Click” above.
If you have been overly stressed (hyperstimulated), you can experience symptoms of any type, number, duration, intensity, and frequency, and at any time. Worrying, fretting, and imagining “the worst” activates your stress response. This is often called “fight-or-flight” but in our modern era, it’s really “fight-or-flight-or-fright” – and the last one is key these days!
For pilots, “flight” is what we want to do. We have little time for “fight” or “fright.” But we live in a stressful world. How we perceive and relate to that stress – unable to flee or to fight – can mean we get trapped into an anxiety pattern we don’t understand and for which we have little training to handle. Certainly flight duties are among the most demanding, from pre-planning all the way through to final parking. Other careers have similar demands, including ship and barge captains, railroad engineers, truck drivers, physicians and surgeons, and many more who must provide exceptional, safe, and effective performance every time, every day, with a high stress tolerance.
Anxiety is one of the most common “mental issues” with which we all deal as adults. Perceived threats can often feel like actual threats to our well-being, even though there may be no real harm. You can experience a physical response, like a racing heart, sudden perspiration, a knot in your stomach, nausea or even vomiting, muscle tension, restlessness, fatigue, difficulty focusing, irritability and mood changes, or inability to sleep and other sleep disturbances. Anxiety can be described in terms of intensity, frequency, duration, degree of interference with duties, triggers, and effects upon you life as a whole.
Anxiety symptoms vary from person to person, often vary over time, and they can grow in severity based on the cause of stress. You could be days and even weeks after a major stressor and still experience the effects of stress. Your symptoms can come and go even though you don’t feel stressed at that moment. With regard to pilots and many others in demanding careers, medications are simply not an answer: indeed, they pose serious performance risks to self and others. Understanding anxiety and daily life stressors can help you to see a better and life-enhancing solution.
Quick explanation: Since you are alive, you have a certain background level of “readiness” to respond. A “stressor” is anything that requires you to respond – it could be as simple as a ringing phone, a knock at the door, or a memory flashing through your mind. You increase your ability to respond by “marshalling forces,” getting into a position to better handle the situation. That is your “alarm” phase. As you work through the situation, that is your “adaptation” phase. As you respond and settle your concern, that is your “resolution” phase – and you return to “baseline readiness,” ready to address the next stressors.
So long as your stressors are minor inconveniences, you generally can handle them well. When your stressors “stack up” in greater number, you might not feel you have the resources to readily respond. Or when your stressors involve more catastrophic challenges, you might feel swamped without enough adaptation resources. This condition is called “overwhelm” and you can suffer ever more extreme symptoms: panic attacks with your heart pounding and racing, shortness of breath, choking, weakness, pains, and even more.
When you fail, for whatever reason, to muster enough resources to resolve these overwhelming stressors, you don’t get resolution but instead fall through your earlier “normal” level of baseline readiness to a new lower zone. You are losing ground, often suffering with a generalized anxiety through each day, and you will feel less able to handle other stressors as they arise.
While our society considers anxiety and stress management to be “mental” issues, these both reflect biochemical changes where your adrenal (stress-response) glands are challenged. That simply means that you can have available nutritional supplements that can dramatically improve your condition and raise your readiness reserves. Certainly that’s not all – using simple prayer and meditation techniques, you can harness the “centering” that will give you ever greater strength, ability, and lasting peace. My experience helping patients cope better in their for lives has given me priceless perspectives over almost 4 dozen years. These and other valuable “hacks” are available to you now when you “Click” above.
Visual changes can be frustrating for everyone, and especially for pilots who need to be alert and aware at all times. Sometimes vision disturbances develop so gradually that you are not aware of your decreased perception … and maybe impaired performance. Extended focus on cockpit instruments and screens can lead to eye strain or visual fatigue, reducing a pilot’s ability to monitor flight data effectively.
“Refractive” testing is done such as for glasses or contact lenses, to help with reading or with distance or both. Several operations have been developed to adjust corneal shape at the front of your eye, but rarely these can create problems that interfere with pilot performance. Evaluation for clouding of the lens – called cataract – might lead to lens replacement, which can be a very successful permanent improvement. Checking the pressure inside your eyeball (usually with a quick and painless puff of air) can show developing glaucoma (where increases can damage your delicate sensing cells). Detailed examination of the interior of your eyeball can show changes in blood vessels, deterioration of your optic nerve, detachment of your retinal (visual) layer from the supporting framework, even clouding or “floaters” in the fluid inside. These tests and others can reveal both localized and systemic disease problems, many of which can be readily corrected.
Here’s where it gets tricky. Despite the unbelievable progress made in the treatment of various eye diseases over the past 50 years, many eye doctors (whether ophthalmologists or optometrists) have little or no appreciation for the incredible contribution that a well-trained integrative medical physician can offer for vision improvement. I asked one of my patients to read the note printed on the outside of a medical chart: “PATIENT IS LEGALLY BLIND.” Then I asked him to read whose chart it was: “Well, that’s MINE!” Yes, his treatments had given him literally a new lease on life. Another patient was thrilled as well – an older lady who was frustrated because she could no longer see well enough to thread a needle, to continue her enjoyment of sewing … she was remarkable better and so satisfied to return to her lifelong hobby. These and other improvements might be available to you as well. If your career or enjoyment of life is at risk, I encourage you to contact my office for personalized care, to see how we might help you recover better sight.
As a group, pilots are generally more concerned and more faithful about taking care of their health. None of us is perfect, that’s for sure. And we have to rely on doctors to give us advice and their guidance might be wrong … or at least, incomplete. Sudden cardiac events (such as heart attack or severe angina pains) are rare. But if they occur in the air, they pose immediate threats to flight safety. The news never fails to share the story of an unfortunate airline captain who has died during the conduct of a flight. The captain passed a first class physical just months ago, so what gives?
Strokes (cerebrovascular accidents) and TIAs (transient ischemic attacks) and even seizures that challenge brain function are likewise rare during flight. But the conditions are certainly set to be challenging: long hours sitting, tight flight deck, continuing mental demands, irregular meals, limited selection of foods, time zone and barometric stress, frequent changes of night lodging, the unexpected demands of weather, equipment, passenger emergencies, and so on. Even in the most healthy among us, years of such stresses can silently take their toll.
Sadly, conventional medical approaches are woefully inadequate in my opinion, which has evolved over almost 4 dozen years of providing effective integrative medical solutions to people suffering with these and similar “untreatable” problems. As a Senior AME for a dozen years, I never had an application for a waiver denied. The reasons are simple:
first, I provided specialized integrative treatments that most often corrected the original
problem such that a pilot’s performance again met expected standards;
then, with my years of surgical and medical experience, I made sure to package with
the pilot’s application all of the tests need for approval … most often, the only “waiver” was for the past episode of whatever, since the pilot had recovered fully and had no need for “allowances” for any “deficient” performance.
These and other improvements might be available to you as well. If your career or enjoyment of life is at risk, I encourage you to contact my office for personalized care, to see how we might help you recover better health and even to return to flight duties for the remainder of your career.
Pay attention! Yes, these kinds of catastrophic health disasters can happen to you, out of the blue. And that could mean that you would be out of the blue skies forever unless you find effective treatment. And that, my friend, is the whole reason for clearedfortakeoff.info!
Cleared for the Approach
Over the course of a flight, pilot capabilities can easily fade due to any number of factors. As cruise leads to approach and landing, task demands rise considerably. Respect these various health conditions so that you take any needed actions to “stay sharp” for when you are most needed to be in control for safe conclusion of your flight.
The FAA has provided an excellent article, worthy of repeated review by all flight crews:
Advisory Circular on Aeromedical Decision Making: AC 60-22: Chapter 4. Stress and Flying
https://www.faa.gov/sites/faa.gov/files/2022-10/AC60-22part2.pdf

You’ll likely find this boring … but I include these details only to reassure you that recommendations based on my extensive background, related experience, and specialized judgment are worthy of your attention.
All said and done, I do have very definite ideas about solving pilot problems …
I didn’t just read about neat ideas, I was chief medical officer for Texas International Airlines before they bought Continental, which ultimately became United Airlines.
I didn’t just read about neat ideas, I was a Senior Aviation Medical Examiner for the FAA for 12 years – I never had an application for a waiver denied – I resigned to do more research on these advanced solutions and hacks I’m sharing with you today.
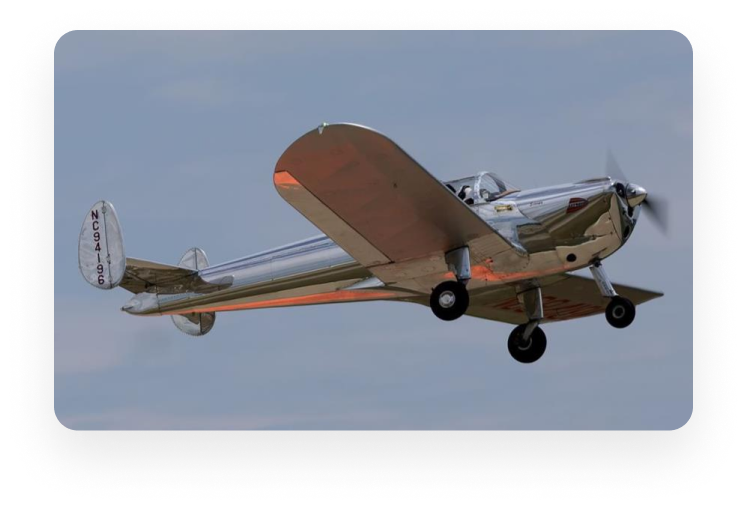
I didn’t just read about neat ideas, I’ve flown 1400 hours all around the county in my antique Ercoupes.
I didn’t just read about neat ideas, I was corporate medical consultant for 53 oil and heavy industry manufacturers in north Houston, for physicals, injuries, and return-to-work rehabilitation.
How’s this: my ideas are better than just general practice prescribing …
I didn’t just read about innovative approaches, after almost 4 dozen years of clinical practice I’ve been recognized as a Marquis Who’s Who Top Doctor in Advanced Medicine.
I didn’t just follow other’s footsteps in a well-beaten trail – in my pioneering career of developing better ways, I am listed in over five dozen volumes of Who’sWho and I received the Marquis Who’s Who Lifetime Achievement Award.
I’ve been more than just a dues-paying member – my professional colleagues have bestowed upon me the distinction of Fellow of the American College for Advancement in Medicine … and also the Distinguished Lifetime Achievement Award of International College of Integrative Medicine … and as more than just an aside, Chairman of the Board of the National Health Federation.
I didn’t just dream up good ideas, I’ve produced over five dozen CDs and DVDs on various topics in integrative medicine (www.healthCHOICESnow.com) and I lectured at airshows for years on how to regain and maintain your medical.
I don’t just “talk” about my innovative practices, I’ve written hundreds of brochures, dozens of articles, and several books – and unlike what we’ve become used to, I have never needed to change a word – among them are …
The Yeast Syndrome – Bantam Books continuing bestseller (since 1986)
Sick and Tired – 2017 update to The Yeast Syndrome Do What You Want To Do – treating all joint pains without surgery
Chapters in bestselling books including with these authors …
Jack Canfield famous for the Chicken Soup for the Soul series,
Internationally acclaimed author/speaker Brian Tracy,
and None other than the iconic media host Larry King.
Ascending to the Flight Levels: paramount recognition as the featured cover article in the preeminent journal, the Townsend Letter: “Still Missing Diagnosis of the Yeast Syndrome?”
Do I really have “new ideas” on many topics …
I didn’t just read about them, I’ve discovered, developed, and shared better solutions with doctors around the world – my original research on so-called “sleep apnea” since 1993 has solved many problems without CPAP.
I didn’t just hear continuing medical education lectures, I have served as program chairman or professor-in-chief for over 2 dozen professional programs and I have given dozens of invited lectures to doctors and patients around the United States, Canada, Mexico, Brazil, and Taiwan.
I didn’t just have tunnel vision to rely only on my earlier training, I was awarded a Diplomate in Preventive Medicine for master’s level studies in nutritional medicine (Medical Research Institute, Florida Institute of Technology).
I didn’t just limit my intensive studies to a small pie-slice of human ailments, I served not only as president of the International College of Integrative Medicine but also as president of the International Academy of Biological Dentistry and Medicine and …
I have gained internationally-recognized credentials in detoxification treatments (chelation therapy) to remove toxic heavy metals to help reverse degenerative diseases of heart/brain/other organs as well as in non-surgical treatments for sports/accidents/other injuries and all joint/neck/back pains.
I didn’t just read about Metabolic Syndrome/”Pre-diabetes” – the discoverer was a friend of mine since 1968 at Stanford. I didn’t just join in beating the drums for “INFLAMMATION,” I was one of the first to write about its critical role in causing all diseases – in 1993!
Others claim “the same” expertise in a number of areas – really?
As a National Merit and California State Scholar, I studied molecular biology at Stanford, graduating with a bachelor’s in biological sciences … and considerable experience in creative writing as well. During my pre-med studies, I assisted with research into making more effective vaccines and undertook graduate courses in immunology. Along the way, I trained as a medical laboratory technologist, receiving the highest certifications (A.S.C.P. and California State), and later I managed quality control for a Kaiser Hospital laboratory.
Half-a-dozen of my professors were Nobel Prize winners – another two dozen were members of the National Academy of Sciences – and I learned advanced literature search strategies at the National Library of Medicine, from the creator of PubMed search. My radiology training was under Harold G. Jacobsen, M. D., in the Bronx – one of the early giants in radiology.
While studying at the Case Western Reserve University School of Medicine, I produced a series of 12 color videotapes on congenital heart disease; my training in blood disorders and cancer was at the National Institutes of Health. Post-graduate studies in general surgery (Mt. Zion Hospital and Medical Center, San Francisco) and urological surgery (kidneys and bladder at The University of Texas, Texas Medical Center, including the M. D. Anderson Cancer Center) gave me surgical perspectives rarely seen in general medical practice.
To further hone my skills in research techniques, I served for 10 years on an FDA-authorized Institutional Review Board, approving applications for clinical studies … or not!
I didn’t just read about this distressing condition needlessly grounding pilots, I was one of the first to popularize understanding of “Auto-Brewery Syndrome” – “drunk without drinking” because gut microbes make alcohol then absorbed into your bloodstream – a totally controllable infection described in my 1986 book, The Yeast Syndrome!
I don’t just “boast a good line,” my career-long successes speak for themselves across so many usual and unusual conditions that steal your health, worsen your suffering, and finally take your life – no matter who claims “advanced” or whatever, there’s no substitute for experience and proven accomplishment.
I seem rather passionate about flying as well as medicine …
First of all, I found my medical training to be sadly lacking – “fighting disease” rather than “restoring better health.” So – I’ve spent a lifetime learning ways of promoting health, realizing that your body functions very much like an airplane, it does just exactly what it is supposed to do in the situation.
Second, I didn’t just watch planes flying overhead, I felt them in my bones: my Dad was a B-36 command pilot, and the Air Force base often vibrated with engine run-ups for hours before launch.
Third, reading Wolfgang Langewiesche’s outstanding classic, Stick and Rudder, during my ground school studies, I was entranced by his description of the “safety airplane” – that was the non-spinnable Ercoupe just being marketed in 1940. (Yes, the very first time I saw one, I bought it … on credit!)
Finally, I have enjoyed “basic flying” in my Ercoupes so much since 1977, I made it my mission to keep as many pilots flying safely as possible. Serving as an Aviation Medical Examiner (Senior for 12 years), I never had an application for a SODA/”waiver” ever rejected, thanks to patient recoveries with my innovative integrative “medical”/health approaches that I now share with you!
Like what you see? – Want me to become your doctor?
Certainly, if you’re interested in a future of optimal health regardless of your current situation – you can visit in person near Houston or you can schedule a teleconsultation to start (and even continue) management. Just
DIAL 1-800-FIX-PAIN
(1-800-349-7246) to start your planning with one of our Treatment Consultants!
Share this with your friends … so they too are CLEAREDFORTAKEOFF (dot)(info)!
And there you have it – “Over to departure, g’day!”
LEGAL LIMITATIONS AND AMAZON AND OTHER AFFILIATE DISCLOSURE NOTICE: The material on this website is presented for general information purposes only and is not a substitute for professional medical or other advice. Be aware that health and medical regulations and aviation practices can differ dramatically across the nations and over time as progress occurs. You should not rely upon the material or information as a basis for making any medical, legal, business, or other personal decisions. Presentation of medical or health-related information does not establish a doctor-patient relationship; you should confirm any proposed action with your personal physician. Information provided has not been evaluated by the United States Food and Drug Administration. In no way are any of the recommendations intended to prevent, detect, treat, or cure any health problems or medical conditions and, as always, individual results will vary.
This disclaimer absolutely limits liability of website owner against any claims regarding any damage or loss caused by your reliance on or use or misuse of any advice, products, content, or omissions or errors herein. You take full responsibility for any potential consequences and you shall indemnify, defend, and hold harmless this website and all associated with it. And further, this website, its owner, and all others associated with it are not responsible for any claims, costs, or damages that might arise from the use or misuse of any website content. And further, this website, its owner, and all others associated with it are not responsible for any warranties, expressed or implied, regarding the use of any products or website content.
This website is a participant in Amazon and other affiliate programs, providing a means for website owner to earn commissions from sales of qualifying product recommendations. Endorsements are unbiased and rely largely on past experience as well as determination of best value; in no case are they influenced by whether you purchase any products through these links.
Certain materials are copyright and are clearly indicated so. Other items may represent permitted “fair use,” citation, or incorporation of another’s protected material. While many comments are based on dozens of years of medical practice experience, no guarantee can be made for the validity of any statements or the results of any proposed action. By offering the information herein, owner has assumed no obligation to provide specific patient care directly or indirectly. Neither reliance on any recommendations nor attempt to embrace any “protocols” or other “specifics” establishes a doctor-patient relationship.
Texas law will be used to settle any disputes that arise from reliance on or use of any content in this website. If any part of this disclaimer is found to be unenforceable, the remaining parts of the disclaimer shall remain in effect. While the owner and webmaster make reasonable efforts to find and fix any mistakes, omissions, errors, or broken links, and to provide current information in continually evolving areas, no guarantee of accuracy can be made. This website is owned by and managed under the direction of LCH-01 [Life Celebrating Health Association], 9816 Memorial Blvd., Suite 205, Humble, Texas 77338.
Privacy and Cookie Policy: Any email address or other information collected about visitors is kept strictly confidential, always protected, and never sold or provided to others. This site might, with your permission, store cookies for your convenience on returning. Please check your preferred choice in the box below:







Select whichever ones interest you:
The most inspiring aviation poem ever written – details you never knew but will forever relish
Stuff for hours of hangar flying discussions, I’ll be adding materials to address these in coming months and years – Please feel free to send me your suggestions and hacks!